Community Diagnostic Centres 10 Human Factors / Ergonomic principles
Select the read more links for more information about that principle and examples of the supporting data.
Community Diagnostic Centre (CDC)
There is a need for expanding diagnostic capacity in the NHS. CDCs can relieve pressure on acute sites and bring services closer to the patient.
The ten principles below represent an accessible way for including systems thinking in the design of the diagnostic workforce and CDC services.
Background: 10 Principles for design
A Human Factors / Ergonomics (HF/E) analysis was undertaken utilising a case study approach in a London community cardiac diagnostic service to contextualise lessons for design.
10 Human Factors / Ergonomics principles are described to provide an accessible way for including systems thinking in the design of community diagnostic centres.
The 10 principles involve systems analysis (IDENTIFY), systems improvement (IMPROVE) and organisational learning (ADAPT).
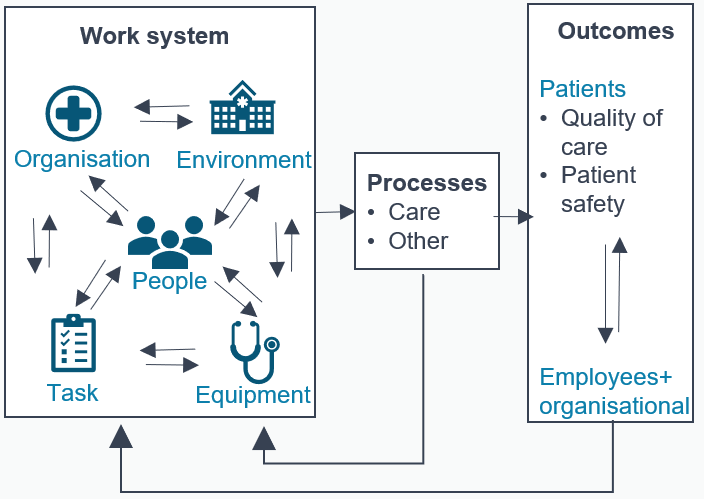
A system perspective
Healthcare is a sociotechnical system - whereby people interact with one another in pursuit of shared goals where they use:
- Tools and equipment
- Engage in tasks
- Are governed by organisational procedures and rules
- Move and work in a physical environment of specific characteristics
These interactions within the work system produce the care processes and outcomes
Background: Human Factors and Ergonomics
Human Factors and Ergonomics is a scientific discipline that is concerned with the design of sociotechnical systems to improve overall system performance, safety, and the wellbeing of people.
- Interactions: HF/E considers the interactions of people with other elements of the system because outcomes are produced by these interactions rather than by any single element in isolation.
- Design: HF/E aims to improve outcomes through system design rather than by telling people to behave differently.
- Human well-being and overall system performance: HF/E considers a broad range of outcomes, including human well-being and quality of working life (e.g., satisfaction, stress, fatigue), and system performance (e.g., safety, effectiveness).
* HOLDEN, R. J., CARAYON, P., GURSES, A. P., HOONAKKER, P., HUNDT, A. S., OZOK, A. A. & RIVERA-RODRIGUEZ, A. J. 2013. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics, 56, 1669-1686
Identify
Understand people's needs and capabilities
- Who is involved?
- What are their goals?
- What are their characteristics?
Consider tools and equipment
-
- What is it going to be used for?
- How is it going to be used?
- Where is it going to be used?
- How easily can it be moved, maintained, cleaned and stored?
-
- Who is going to use it?
- What are the user's characteristics, capabilities, and needs?
- How easy is it to understand and use it?
-
Analyse organisational structures and processes
-
- Procurement
- Workforce planning
- Estates and infrastructure planning
- Attitudes towards risk and safety
-
Improve
Promote autonomy and professional growth
- Equitable access to career progression and recruitment
- Effective training and supervision across organisations
- Flexible skill mix and staff mobility
- Psychologically safe environment
Focus on the needs of patients in the community
- Access to diagnostic services quicker and closer to home
- Enhance diagnostic capacity in primary care
- Tailor to local contexts
Facilitate communication across organisations
-
- Effective transfer of information across systems and services
- Consider the diverse needs of different stakeholders
-
- Optimise digital communication
- Embed digital communication technologies in well-designed processes
-
Adapt
Monitor work-as-done and adapt to achieve sustainable change
- Continuous learning process
- Agile and adaptive approach

The CIEHF organisational learning framework for achieving sustainable change. Record and learn from feedback and events
-
- Adverse events and incidents
- Patient experience feedback
- Patient behaviours
- Staff concerns and experience feedback
- Staff behaviours
-